Wound
Wound care
Bacteriostatic Wound Dressing
Products – Hydrofera
References (Case Studies)
Where to Buy
HydroGel
Available in gels, gel covered gauze, or sheets, hydrogel wound dressings require a second dressing to maintain moisture and promote wound healing. Hydrogels offer cooling effects to relieve pain and discomfort. This type of wound dressing is best for wounds with light drainage.Application of hydrogels is contraindicated when the wound is producing moderate to heavy exudate because if the wound is very wet, the presence of the hydrogel would contribute to wound maceration. If a wound is infected, application of most hydrogels serves no real purpose since plain hydrogel products do not contain an antimicrobial agent.
Hydrogel sheet is non-adhesive and will not stick to the wound bed. It keeps the wound moist, protects the wound against contamination, is capable of absorbing some exudate and promotes healing. It is secured to the wound using a secondary dressing such as a biocclusive type of covering
These should be used as a primary wound dressing choice in wounds that are substantially or fully granulated. If there is a great deal of black eschar or yellow or white slough, the wound should be enzymatically debrided or sharps debrided to remove the necrotic tissue.
Hydrocolloid
Hydrocolloid dressings, adhesive wafer dressings stick directly over wounds and form a gel-like substance when the gelling agents in the dressing interact with drainage from the wound. The gel substance makes an ideal environment for a healing wound.
Characteristics & Uses : Hydrocolloid dressings contain a dressing matrix which absorbs exudate and creates a gel like dressing. The gel may be retained inside the dressing where the matrix is located or the hydrocolloid gel may be formed in the wound. These dressings help the wound to autolytically debride itself.
The hydrocolloid dressing is impermiable to water vapor, oxygen and bacteria. These dressings are not adherent to the wound bed and can be removed without tearing the granulation tissue underneath. They are best applied to wounds that produce light to medium exudate or transudate. If the wound is not too wet, these primary dressings may remain in place for 3-4 days. These dressings can be placed on wet wounds and wet surronding skin and will remain intact because they can adhere to a moist area - a feature called wet tack.
Disadvantages : These dressings should not be applied over infected wounds. They should not be applied over wounds that are producing moderately heavy exudate. These dressings can develop a foul odor to them after having been applied for 2-4 days. Sometimes when they are removed, clinicians think the wound has become infected when, in fact, the odor is coming from the hydrocolloid dressing.
Alginates
 Alginates get their name because they are derived from kelp and other brown seaweeds. Alginates turn into a non-sticky gel when placed over a draining wound. Gauze or larger bandages hold the alginates into place above a wound and prevent the alginate from drying out as rapidly. Placing the alginates in layers provides more absorbency and ensures the alginates stay wet longer.
Alginates get their name because they are derived from kelp and other brown seaweeds. Alginates turn into a non-sticky gel when placed over a draining wound. Gauze or larger bandages hold the alginates into place above a wound and prevent the alginate from drying out as rapidly. Placing the alginates in layers provides more absorbency and ensures the alginates stay wet longer.
Characteristics & Uses : Alginates fibers are soft in texture and are easily pulled apart without any difficulty. The alginate dressings are considered to be primary dressings for wounds that have moderate to heavy exudate and transudate. Generally they are placed in wound beds for the purpose of absorbing exudate or transudate and keeping the wound moist. The alginate, once wet with exudate, forms a gel-like plug in the wound. The alginate can absorb up to 20 times its weight in exudate. It facilitates autolytic debridement of the wound and generally has to be held in place by a secondary dressing such as a biocclusive thin film, a hydrogel sheet, or gauze.
Alginates are most often lifted out from the wound or irrigated and washed free from the wound bed when a dressing is being changed. They do not adhere to the wound bed surface and therefore do not debride the wound when removed. One very nice feature of the alginates is the ability to leave them in the wound - they do not have to be removed from the wound during dressing changes because they do not cause increased inflammation or irritation to the wound. When a wound has a deep and extensive undermined region or has a number of tunnels, the alginate can remain behind without any fear of causing infection. The body will dissolve and absorb the alginate if it remains in deep cavitations, tunnels or undermined areas. See the picture below.
Disadvantages Of Alginates : Alginates should not be wet with normal saline or sterile water before being placed in the wound bed. Wetting the alginates defeats the purpose in using them in a wound. Also, alginates should not be used in dry or dessicated wounds.
Foams
 Used often on new wounds, foam dressings absorb large amounts of fluid and wound drainage. Some foam dressings come with adhesive backings while others require gauze wrapping to stay in place.
Used often on new wounds, foam dressings absorb large amounts of fluid and wound drainage. Some foam dressings come with adhesive backings while others require gauze wrapping to stay in place.
Foam dressings are highly absorbant primary dressings usually made of a hydrophilic polyurethane foam. These dressings keep a moist wound environment but absorb the excess exudate sometimes seen in wounds. These dressings are useful for cavitating wounds because they can be placed in the wound to fill the wound bed while absorbing the continuous exudate seen in wounds during the inflammatory phase of wound healing. The foam dressings which are placed in deep wounds can remain for 3-4 days and must be secured in place by a biocclusive type dressing. Some of the foam dressing products have an adhesive backing at the margins of the dressing and therefore these cannot be packed into deep wounds. Foam dressings with adhesive backings are very useful for placing over wounds smaller than the absolute diameter of the dressing.
- Transparent Film
Moisture Vapor Permeable Films
Characteristics and Advantages
Characteristics and Advantages
Moisture vapor permeable film dressings are adhesive film dressings that are waterproof but which are also semi-permiable to the passage of oxygen and water vapor to and from the wound site. These dressings prevent the wound from dessication as well as from contamination by bacteria. They help maintain a moist wound healing environment and retain growth factors next to the wound bed that are in the exudate and transudate. These dressings also promote autolysis of necrotic tissue in the wound bed.
These film dressings are translucent or clear and help the wound care clinician to visualize the wound. They can be placed over areas that are somewhat difficult to bandage because they are very thin, flexible and have an adhesive backing.
Uses
These dressings are good secondary dressings over wounds in areas where there may be a good deal of shear such as the elbows, heels, iliac crest, knees, and wrists. MVPF dressings adhere better to the skin over wounds that are producing light to medium exudate. MVPF dressings may be left in place for several days in wounds that are not infected and which are not continually producing lots of exudate. In wounds that are producing heavy exudate, they will need to be changed more often and may become so wet as to lessen the effectiveness of the adhesive causing them to easily be rolled off the area of application with very little shear or frictional force.
These dressings are especially good when they are applied over wounds in which a primary dressing must be held in place. The application of alginates into a wound bed can be retained in the wound bed very efficiently with the application of a thin film dressing.
- Anti Bacterial / Antimicrobial / Bacteriocidal
An antimicrobial dressing is a wound dressing which is designed to inhibit the growth of microbes in and around the wound. Such dressings are utilized in cases where there are concerns about infection and care providers would like to limit opportunities for infectious agents to colonize a wound site as much as possible.
Chronic wounds are characterized by high bacterial count, the presence of more than one bacterial strain, tendency to harbor more drug resistant organisms and presence of biofilms. The presence of infections is highly detrimental to the wound healing process.
The dressing may have a foam, fabric, film, sponge, or gauze base. It is impregnated with an agent which inhibits microbial growth. When applied to a clean wound, the antimicrobialdressing will prevent microbes from growing on the wound and bandage, keeping the patient more comfortable.
It is now known that a moist wound environmentis more conducive to healing than a dry one. The use of moisture-retentive dressings has become the norm, and these dressings have been shown to shorten healing time in various types of wounds. However, with added moisture in wounds there is also the creation of an environment that is conducive to the growth of bacteria.
Many wounds, particularly chronic long-standing wounds, have some degree of bioburden. In fact, this is almost expected, and clinicians pay little attention to this fact unless critical colonization, and a resultant slowing of the healing process, is noted; wounds that have a heavy bioburden along with signs and symptoms of infection are generally treated with some form of antimicrobial therapy. Antimicrobial dressings have become one weapon in the arsenal of antimicrobial therapy.
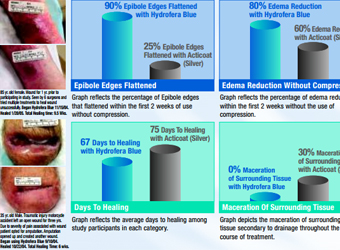
Antimicrobial dressings work by slowly releasing their active ingredient into the wound bed. In doing so, it is hoped that they will neutralize (kill) bacteria while having little effect on healthy cells. While there is one dressing Hydrofera Blue which sucks out the exudates from the wound bed and kills the bacteria in the dressing itself without releasing any active anti bacterial agent on the wound bed.
Hydrofera Blue® - Antimicrobial Wound Dressings
PVA Sponge Dressing pigmented with Methylene Blue and Gentian Violet
Hydrofera Blue is a simple, safe, effective and proven moist wound dressing. It is constructed of polyvinyl alcohol (PVA) sponge complexed with two organic pigments, which provide broad-spectrum Antimicrobialprotection. The pigments (Methylene Blue and Gentian Violet) have been used safely in medicine for over 50 years and have proven effective against a variety of microorganisms including MRSA and VRE.
Dressings containing silver
There are many dressings on the market that use silver. Silver has been incorporated into numerous dressing types, such as foam dressings, alginate dressings, gauzes and films. They may be used as a primary or secondary dressing. They can be very absorptive, depending on the type of dressing chosen. Silver has been shown to be able to kill numerous organisms.
Disadvantage , however with silver is that, it may not be as highly effective in wounds containing multiple organisms or on biofilms.
Dressings containing silver are recommended for use on wounds that are critically colonized or infected. There is no evidence supporting their use in wounds that are not infected as they have not been shown to speed healing in these wounds. Silver dressings are more expensive than other dressings and vary greatly in the type and amount of silver released. Clinicians should carefully read directions for use and should keep in mind that saline will deactivate the silver in some cases. In addition, patients with a silver dressing should have their dressing removed before undergoing an MRI.
Iodine dressings
Iodine has been used for many years as an antimicrobial, but has only been introduced in dressing form in recent years. Cadexomer iodine is the form of iodine commonly used in dressings. It is indicated for use in chronic wounds which are thought to be, or known to be, infected.
Disadvantage being that these cannot t be used on patients who have a hypersensitivity to iodine and should also not be used in patients with thyroid disease due i.e. thyroiditis, goiters as it is absorbed systemically.
Polyhexamethylene biguanide
Polyhexamethylene biguanide (PHMB) has shown to be an effective antimicrobial against a wide array of human pathogens, including HIV. It acts by disrupting cellular membranes in bacterial cell walls. It is indicated for use on partial- and full-thickness wounds, exudating or dry. This dressing has been shown to decrease wound pain.
Disadvantage being that, while PHMB is effective against the bacteria it comes in direct contact with, it is less effective at dispersing beyond the wound bed to the periwound.
Over all disadvantage of Anti bacterial dressings is that these are not currently recommended for uninfected wounds and should only be used on wounds that are critically colonized or infected. They should be used for the shortest time required and should be discontinued if there is no improvement in wound appearance and healing within two weeks of beginning therapy. In addition, clinicians should keep in mind that indiscriminant use ofantimicrobial dressings may lead to resistant bacteria.
THIS DISADVANTAGE IS NEGATED BY THE USE OF Hydrofera Blue® - Antimicrobial Wound Dressings since the active anti microbial agent is not released on to the wound bed but the all the anti bacterial activity takes place with in the dressing itself.