Wound
Wound care
Bacteriostatic Wound Dressing
Products – Hydrofera
References (Case Studies)
Where to Buy
What is a Wound?
A wound may be described in many ways; by its aetiology or cause , anatomical location, by whether it is acute or chronic1, by the method of closure, by its presenting symptoms or indeed by the appearance of the predominant tissue types in the wound bed. All definitions serve a critical purpose in the assessment and appropriate management of the wound through to symptom resolution or, if viable, healing.
A wound by true definition is a breakdown in the protective function of the skin; the loss of continuity of epithelium, with or without loss of underlying connective tissue (i.e. muscle, bone, nerves) following injury to the skin or underlying tissues/ organs caused by surgery, a blow, a cut, chemicals, heat/ cold, friction/ shear force, pressure or as a result of disease, such as leg ulcers or carcinomas.
Wounds heal by primary intention or secondary intention depending upon whether the wound may be closed with sutures or left to repair, whereby damaged tissue is restored by the formation of connective tissue and re-growth of epithelium
Structure and Function of the Skin
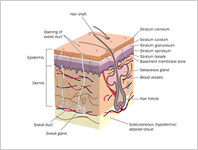 The skin is one of the largest organs in the body in surface area and weight. The skin consists of two layers: the epidermis and the dermis. Beneath the dermis lies the hypodermis or subcutaneous fatty tissue. The skin has three main functions:protection, regulation and sensation. Wounding affects all the functions of the skin.
The skin is one of the largest organs in the body in surface area and weight. The skin consists of two layers: the epidermis and the dermis. Beneath the dermis lies the hypodermis or subcutaneous fatty tissue. The skin has three main functions:protection, regulation and sensation. Wounding affects all the functions of the skin.
The skin is an organ of protection. The primary function of the skin is to act as a barrier. The skin provides protection from: mechanical impacts and pressure, variations in temperature, micro-organisms, radiation and chemicals.
The skin is an organ of regulation. The skin regulates several aspects of physiology, including: body temperature via sweat and hair, and changes in peripheral circulation and fluid balance via sweat. It also acts as a reservoir for the synthesis of Vitamin D.
The skin is an organ of sensation. The skin contains an extensive network of nerve cells that detect and relay changes in the environment. There are separate receptors for heat, cold, touch, and pain. Damage to these nerve cells is known as neuropathy, which results in a loss of sensation in the affected areas. Patients with neuropathy may not feel pain when they suffer injury, increasing the risk of severe wounding or the worsening of an existing wound.
Wound Healing Process
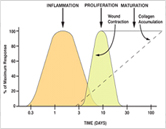 Whether wounds are closed by primary intention, subject to delayed primary closure or left to heal by secondary intention, the wound healing process is a dynamic one which can be divided into three phases. It is critical to remember that wound healing is not linear and often wounds can progress both forwards and back through the phases depending upon intrinsic and extrinsic forces at work within the patient.
Whether wounds are closed by primary intention, subject to delayed primary closure or left to heal by secondary intention, the wound healing process is a dynamic one which can be divided into three phases. It is critical to remember that wound healing is not linear and often wounds can progress both forwards and back through the phases depending upon intrinsic and extrinsic forces at work within the patient.
The phases of wound healing are:
- Inflammatory phase
- Proliferation phase
- Maturation phase
The inflammatory phase is the body’s natural response to injury. After initial wounding, the blood vessels in the wound bed contract and a clot is formed. Once haemostasis has been achieved, blood vessels then dilate to allow essential cells; antibodies, white blood cells,growth factors, enzymes and nutrients to reach the wounded area. This leads to a rise in exudate levels so the surrounding skin needs to be monitored for signs of maceration. It is at this stage that the characteristic signs of inflammation can be seen; erythemea, heat, oedema, pain and functional disturbance. The predominant cells at work here are the phagocytic cells; ‘neutrophils and macrophages’; mounting a host response and autolysing any devitalised ‘necrotic / sloughy’ tissue.
During proliferation, the wound is ‘rebuilt’ with new granulation tissue which is comprised of collagen and extracellular matrix and into which a new network of blood vessels develop, a process known as ‘angiogenesis’. Healthy granulation tissue is dependent upon the fibroblast receiving sufficient levels of oxygen and nutrients supplied by the blood vessels. Healthy granulation tissue is granular and uneven in texture; it does not bleed easily and is pink / red in colour. The colour and condition of the granulation tissue is often an indicator of how the wound is healing. Dark granulation tissue can be indicative of poor perfusion, ischaemia and / or infection. Epithelial cells finally resurface the wound, a process known as ‘epithelialisation’.
Maturation is the final phase and occurs once the wound has closed. This phase involves remodelling of collagen from type III to type I. Cellular activity reduces and the number of blood vessels in the wounded area regress and decrease.
Wound Classification
The classification of wounds, supports good assessment and helps in planning the correct treatment course for the fast wound healing. Apart from this the classification also assists with continuous reassessment and evaluation of the results of the treatment regimen being followed.
Wounds can be classified with respect to the following common criteria’s:
- Description
- Wound age
- Wound depth and tissue loss
- Wound color
- Drainage
- Wound bed
- Cause/Indication :
Types of Wounds
Fungating Wounds
Fungating lesions are known as ‘masses’ or ‘ulcerative lesions’ and are a result of cancerous cells infiltrating epithelial tissue. The management of patients with a fungating wound is focused essentially upon symptom control and appropriate psychosocial support. They pose a problem for both patients and healthcare professionals as they signify progressive and life threatening disease and affect quality of life by causing unpleasant and difficult to manage symptoms
The main presenting symptoms for a fungating wound are:
- Pain
- Malodour
- Heavy exudate
- Peri-wound excoriation
- Capillary bleeding
- Local Infection
Dressings should be selected which manage the patient’s symptoms and:
- Reduce / eliminate wound malodour
- Manage and treat wound infection
- Manage wound exudate and protect the peri-wound area
- Provide haemostasis
- Manage the tissue types at the wound bed
- Facilitate atraumatic dressing changes
- Improve quality of life / reduce social isolation
- Are comfortable and aesthetically pleasing for the patient
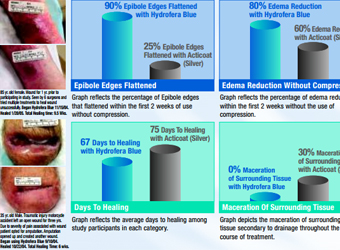
Hydrofera Blue Wound dressing is an ideal dressing which can manage all the symptoms of these wounds except providing heamostasis action.
Leg Ulcers
Leg ulceration has commonly been defined as ‘a loss of skin below the knee on the leg or foot which takes more than six weeks to heal.
The majority of leg ulcers are caused by Venous Disease (70%), the remainder by either peripheral Arterial Disease (20%) or as a result of mixed aetiology or cause, skin malignancies, metabolic disorders such as Diabetes, rheumatoid disorders, dermatological conditions or are self inflicted (10%). Most elderly patients who present are mulitfactorial.
Appropriate management of the leg ulcer is dependent on a holistic assessment of the patient, the limb and the ulcer. Medical and surgical histories should be reviewed and both intrinsic and extrinsic risk factors considered. The aetiology of the ulcer should then be determined by using a Doppler and the ABPI (Ankle / Brachial Pressure Index) calculated.
The ABPI detects arterial insufficiency. False readings can occur in patients with Diabetes or Atherosclerosis. This assessment should always be conducted by a trained healthcare professional, an inaccurate assessment and diagnosis could be detrimental for the patient.
On assessment; venous and arterial ulcers often present differently in appearance. Venous Ulcers may be: Shallow in appearance and situated around the ‘gaiter region’ of the leg, oedematous, there may be ankle flare and hyper pigmentation (brown staining) and the leg may be ‘hardened‘. Arterial Ulcers may present as being: ‘punched out’ in appearance, poorly perfused, the legs and feet are cool to touch and there may be gangrene to the toes, the leg is often shiny, hairless and the skin may be tight.
Dressings should be selected which manage the presenting conditions at the wound bed and optimise patient comfort. The wound should be assessed for the presence of infection, however many ulcers are colonised by microorganisms due to their chronicity. Many ulcers are malodorous due to the presence of the microorganisms, which have colonised the ulcer bed, in particularly bacterial species such as Pseudomonas aureginosa.
Leg ulcers, if they are venous in aetiology may be treated with compression therapy; multi-layer / short stretch bandaging and / or hosiery. The key is to ensure clinicians have the knowledge and experience to apply the bandages correctly. Once the ulcer is healed the patient should continue in compression hosiery to prevent reoccurrence.
The Hydrofera Blue wound dressing is ideally suited since it be worn under the compression bandages required for treating venous ulcers, The Methylene Blue & Genatin violet the active ingredients of the Hydroferra kill most of the microorganisms that can colonize the Leg ulcers, including the Pseudomonas aureginosa. Moreover Hydrofera Blue can even self debride and remove the Biofilm formed on these wounds.
Diabetic Foot Ulcers
Diabetic foot ulceration poses a major challenge to health professionals involved in the management of diabetes; a multidisciplinary approach leads to good preventative care and appropriate timely wound care intervention.
Patients with a diabetic foot ulcer need to be assessed holistically and intrinsic and extrinsic risk factors considered. Key patient risk factors include; blood glucose levels, peripheral vascular disease, neuropathy, limited joint mobility, foot deformity, callus, and medication, smoking and visual impairment.
There are principally two types of the ‘at-risk’ foot; neuropathic (90%) and neuroischaemic (10%). The aetiology of the foot ulcer must be determined before treatment plans are put into place. The ulcer should be assessed with regard to severity, location, presence of infection, stage of healing, temperature and odour. Diabetic foot ulcers can be classified; two scales in use are the Wagner Classification and the San Antonio.
The neuropathic foot / ulcer commonly presents with a warm, well-perfused foot with palpable pedal pulses. The foot will not ‘sweat’, is subject to dry skin leading to cracking contributing to excess callus formation and the arch of the foot is commonly raised and the toes may be clawed. Ulceration is commonly found to the sole of the foot underneath neglected callus and high planter pressures.
The neuroischaemic foot / ulcer is cool and pulseless, poorly perfused, the foot can appear deceptively pink and healthy as the capillaries dilate in an attempt to improve the circulation and can appear warm if it is infected. Ulcers are commonly seen on the edge of the foot, the tips of the toes or the areas around the back of the heel. They are usually caused by trauma such as ill fitting footwear.
The diabetic foot ulcer is largely ‘at risk’ of tissue necrosis and severe infection which may result in gangrene. They should be assessed regularly for signs of wound infection, remembering that infected wounds are often minimally symptomatic, displaying only exudate, odour or mild discomfort.
A wound dressing should be selected to support a moist wound environment, prevent further trauma, treat / prevent infection, manage exudate, control odour and protect the peri-wound skin. External pressure can be reduced to the wound with appropriate footwear; bed rest or other ‘offloading’ devices.
Acute Wounds
There are principally two types of acute wound; traumatic wounds and surgical wounds 1.
A traumatic wound such as a minor cut, abrasion through to extensive tissue injuries are caused when a force exceeds the strength of the skin or the underlying supporting tissues. A traumatic wound is classified by whether or not it is tidy or untidy.
A surgical wound is either incised and suture or laid open to heal by a surgeon. The wound breaks the integrity of the skin including the epidermis and dermis. Surgical wounds are classified in relation to the potential for infection in the wound: they are considered to be either clean, clean contaminated, contaminated or dirty. Surgical wounds which are contaminated / dirty or infected are sometimes left open post surgery whilst the infection resolves and then they are sutured closed. This is known as ‘delayed primary closure’. Premature primary closure in these instances can be detrimental to a successful outcome.
Management of a severe traumatic wound initially involves emergency procedures; resuscitation and restoration of the circulation to the affected limb / area. Associated injuries should be considered. The blood supply must be optimised, any necrotic tissue debrided away as this can act as a focal point for bacteria, and the wound irrigated. Antibiotics and tetanus are usually given prophylactically.
The correct intervention can greatly affect the outcome for the patient: the scar, time to heal and quality of life. With any acute wound the post-operative function of the wounded area and adequate pain control is essential. If pain is not controlled adequately it can decrease oxygen uptake, increase mortality and morbidity, delay mobility and increase hospital length of stay.
For these wound types, dressing selection should be based upon absorbing wound exudate, supporting haemostasis and protecting the wound from infection. It is also critical to manage the peri-wound area. Exudate levels can be high during the inflammatory phase and leakage of corrosive exudate onto the surrounding skin under the dressing can lead to ‘blistering’. Protection of the peri-wound area with a ‘no sting’ barrier film preparation such as LBF may be appropriate 2.